Medicare has eliminated the quarterly Dual/LIS Maintaining Special Election Period and replaced it with 2 new SEPs. Dual and LIS beneficiaries will have new restrictions on plan changes, including when they can change, and which plans they can change. Make sure you understand what changes your clients can or can’t make starting January 2025.
What are the new DSNP/LIS Special Enrollment Periods?
Integrated Care Special Enrollment Period
This SEP is for full-benefit dually eligible individuals to make a once-per-month election to join a Dual Special Needs plan. This includes Fully Integrated Special Needs Plans (FIDE SNP), highly integrated dual eligible special needs plan (HIDE SNP), or an applicable integrated plan (AIP). If they are joining a D-SNP plan during this SEP, the new plan MUST align with their Medicaid health plan. This means the D-SNP company must match their Medicaid insurance company. When enrolling in a D-SNP plan during this time, be sure you use this Election Code so it doesn’t get declined.
If they have a different enrollment period, some of these limitations may no longer apply. See below for more information.
Changes that can be made under the Integrated Care SEP:
- Change from MAPD to Aligned D-SNP
- Change from PDP to Aligned D-SNP
- Change from non-aligned D-SNP to Aligned D-SNP
Dual/LIS Special Enrollment Period
This second new SEP is also a monthly SEP that allows one change per month. HOWEVER, individuals are limited in the changes they can make. This SEP allows individuals with any level of Medicare Savings Program and/or Extra Help to either switch between stand-alone PDP plans, or leave their current MAPD plan and return Original Medicare and a stand-alone PDP. This SEP does not allow beneficiaries to join a MAPD or join a D-NSP. This is why it is important to pick the correct SEP name when enrolling a client into a D-SNP using the above Integrated Care SEP.
This means beneficiaries can no longer enroll in any MAPD plan using the DUAL/LIS SEP. Only people eligible for the D-SNP plans listed above can enroll in a new D-SNP plan using the new Integrated Care SEP, but ONLY IF it aligns with their Medicaid plan.
Changes that can be made under this SEP:
- Change from MAPD to Original Medicare & stand-alone PDP
- Change from stand-alone PDP to stand-alone PDP
Please remember, if they have a change in MSP or LIS benefit level then you would use the Dual/LIS Change in Status SEP and not the above listed SEPs. See below on how other enrollment periods may overrule the above SEP limitations.
What if a beneficiary qualifies for a different enrollment period?
The limitations for the Integrated Care and Dual/LIS SEPs are only applicable during these listed enrollment periods (except restrictions for individuals with Long-term Care Benefits). If a beneficiary qualifies for a different enrollment period, including other special enrollment periods, then they can make a normal change. The D-SNP alignment rules are not applicable under other enrollment periods UNLESS they have Long-Term Care (LTC) Medicaid benefits. If they have LTC Medicaid benefits, then their D-SNP plan MUST ALWAYS align with their Medicaid no matter when they enroll. But if they don’t have LTC benefits, then their Medicaid plan does not have to align to their D-SNP plan when using a different enrollment period. This means that all other SEPs and Enrollment periods overrule the Dual/LIS and Integrated Care SEPs requirements!
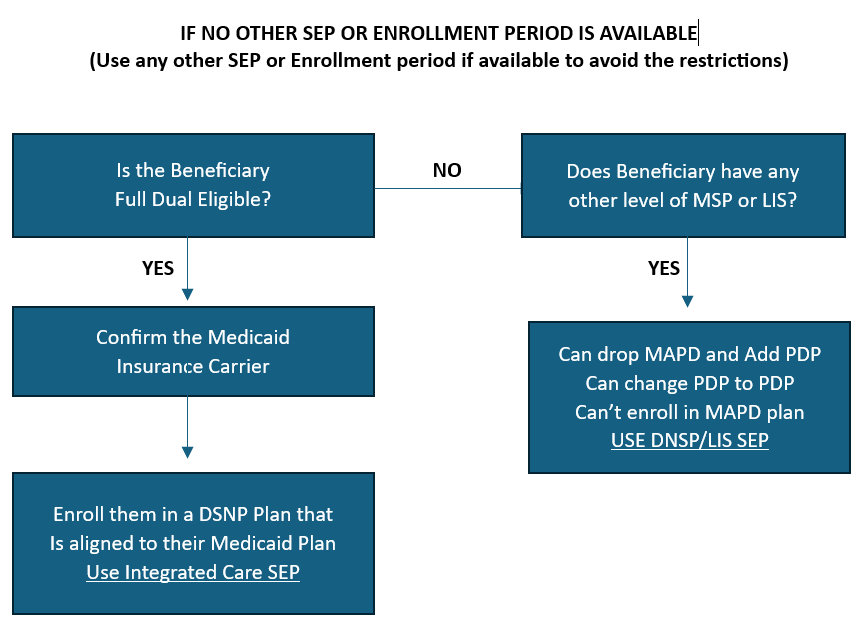
It sounds complicated, but we recommend you use any other enrollment period if it is available to avoid the above restrictions and confusion. If there is not one available, then follow the below guide.
Example of Integrated Care SEP
Marcy is full dual status and qualifies for a Dual Special Needs Plan, but she is currently on a regular MAPD. It is April, so she missed the MAPD Open Enrollment Period to make a change. She can use the Integrated Care SEP to enroll in a D-SNP plan to start next month. Her Medicaid plan is United Healthcare, so the only D-SNP plan she can enroll in during this time is the UHC D-SNP plan. If she enrolls in April, her coverage will start May 1.
Example of Dual/LIS SEP
John currently has a MAPD and receives Extra Help for his prescriptions. He was prescribed a new prescription that is not on his formulary and would like to find a new MAPD plan that will cover it. Because the new Dual/LIS does not allow him to join a new MAPD, he can only use the election to leave his current MAPD and go back to Original Medicare with a stand-alone PDP.
Example of D-SNP change using any other enrollment period
Rebecca current has an MAPD but is fully Dual eligible and just learned about the dual plans. It is February and she wants to join a D-SNP. Her Medicaid insurance is with XYZ Company, but the D-SNP Plan offered by ABC Company gives her more benefits than that D-SNP plan with XYZ Company. Since it is technically the MAPD Open Enrollment, she can use this SEP to enroll in the ABC Company D-SNP plan even though it doesn’t align with her Medicaid carrier, XYZ Company. She does not have to adhere to the Integrated Care SEP rules since she qualifies for a different enrollment period.
If you have questions about these changes, reach out! If you are not already contracted with us and want access to all our great resources for you and your downline then CONTACT US HERE. Don’t miss out on all the benefits of joining our team.
