
Medicare costs can add up for beneficiaries for both prescriptions and medical costs. Even with Medicare coverage, they have a myriad of potential expenses including premiums, co-pays, co-insurance, and prescription drug costs, as well as potential penalties for Part B or Part D. The Extra Help/Low Income Subsidy can help low-income Medicare beneficiaries reduce their out-of-pocket prescription drug costs. It is necessary to understand all the ins and outs of this program to determine if any of your potential or current Medicare clients qualify and what their costs will be once they do. Let’s learn more below!
What is the Low-income Subsidy (LIS)/ Extra Help Program?
Extra Help, also known as Low-income Subsidy (LIS), is a federal program that helps low-income people with Medicare pay for out-of-pocket costs associated with Part D prescription drug coverage. This may include help with monthly premiums, annual deductibles, and co-payments related to the Part D prescription drug program and is estimated to be worth about $5,000 per year.
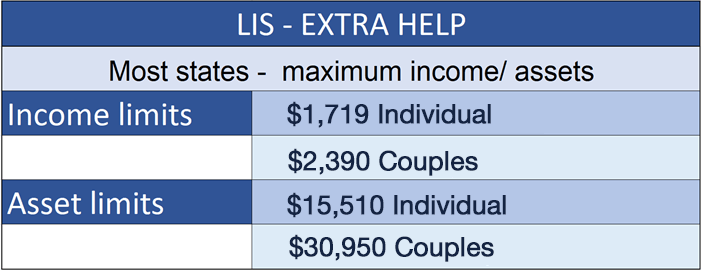
To qualify for Extra Help, a person must be receiving Medicare, have limited resources and income as indicated by the graph below, and reside in one of the 50 States or the District of Columbia.
The level of subsidy depends on the level of income and assets a person has available and can be awarded as either Full LIS or Partial LIS. The Extra Help income test for determining which level of subsidy an individual can qualify for is based on the Federal Poverty Levels (FPLs). But do not assume that a person is not eligible if their income is above the FPL because the maximum income for partial LIS is up to 150% of the FPL. Here are the maximum income and asset levels that a person can have and still qualify for at least partial Extra Help in 2022. The amounts change each year based on each years FPL.
How to apply for LIS/Extra Help
The application for Extra Help is completed with Social Security. The quickest way to apply is online through the Social Security website at https://www.ssa.gov/benefits/medicare/prescriptionhelp/. However, they can also call Social Security at 1-800-772-1213 to apply by phone, request a paper application mailed, or make an appointment at the local Social Security office. Social Security can take approximately 3 weeks to process and make a determination on your application.
When determining which customer’s income falls within the income limits for LIS, not all sources of income may need to be included. Below is a list of income that needs to be included and income that can be excluded.
The following income must be included on the application:
- Social Security benefits (e.g., retirement, SSI), Railroad Retirement benefits
- Pensions or annuities, including veteran’s pensions
- Wages (gross) or earnings from self-employment (net)
- Alimony
- Rental income (net)
The following are excluded from income when applying:
- SNAP (Food Stamps) & LIHEAP (fuel assistance) benefits
- $20/mo in unearned income, such as Social Security
- Housing or home energy assistance
- Assistance from others to pay your household expenses
- Work-related expenses for people who get Social Security benefits for a disability or blindness
- COVID-19: Economic impact payments
Similar with income limits, a beneficiary’s assets cannot be over the specified limits above to qualify for any level of LIS. The following are resources that need to included or excluded when listing resources on the Extra Help application.
Countable resources include:
- Financial accounts (e.g., checking, savings, CDs)
- Cash at home
- Stocks, bonds, savings bonds, mutual funds, individual retirement accounts (IRAs), 401(k) accounts
- Real estate (equity value) other than primary home
- Certain trusts that allow a person to revoke or have direct use of funds
Excluded resources include:
- Home in which the applicant lives
- All vehicles (autos, trucks, motorcycles, boats, snowmobiles, etc.)
- Household goods/furnishings, and personal effects (e.g., jewelry)
- Cash surrender value of life insurance policies
- In-kind support (e.g., non-cash help such as shelter)
- Irrevocable burial trusts/burial contracts
After applying, Social Security will review the application and send a letter letting the beneficiary know if they qualify for Extra Help. People who already have Medicaid do not need to apply for LIS and will automatically qualify and get a letter from CMS letting them know.
Extra Help Application Tip: When applying for LIS, you can opt to start the application process for the Medicare Savings Program (MSP) and the Social Security Administration will sends the application data to the state Medicaid office. MSP helps reduce the out-of-pockets costs of Medicare Part A and Part B.
To learn more about the Medicare Savings Program, check out “The Ins and Outs of the Medicare Savings Programs” blog.
Extra Help/ LIS Annual Review Eligibility
If you applied for Extra Help through Social Security, then you will need to continue to meet eligibility requirements each year. Reviews generally happens in August of each year and you may receive a letter from Social Security if you need to complete a review. If you do not complete your review, or if your review shows you no longer qualify for Extra Help, then your Extra Help will end December 31st. Keep in mind, this does not cancel your Part D Prescription Drug plan. If you anticipate your Extra Help will end, then you should review the Part D Prescription Drug plan you are enrolled to determine what your new out-of-pocket costs will be without the Extra help. It may be a good idea to compare to other Part D Prescription Drug plans at this time.
If you originally automatically qualified for Extra Help because you had Medicaid, Supplemental Security Insurance (SSI), or a Medicare Savings Program (MSP), and you are still enrolled in one of these programs come the fall, then you will not have to do an annual review through the Extra Help program. The state will automatically inform Medicare that you are still enrolled. But if you have lost your status in the Medicaid, SSI, or MSP program then you will get a letter from Social Security stating your Extra Help benefits will end December 31st . If this is the case, you can apply for Extra Help directly through Social Security if your income falls within the eligibility limits and you don’t want your Extra Help benefits to end.
Extra Help/ LIS Coverage Levels
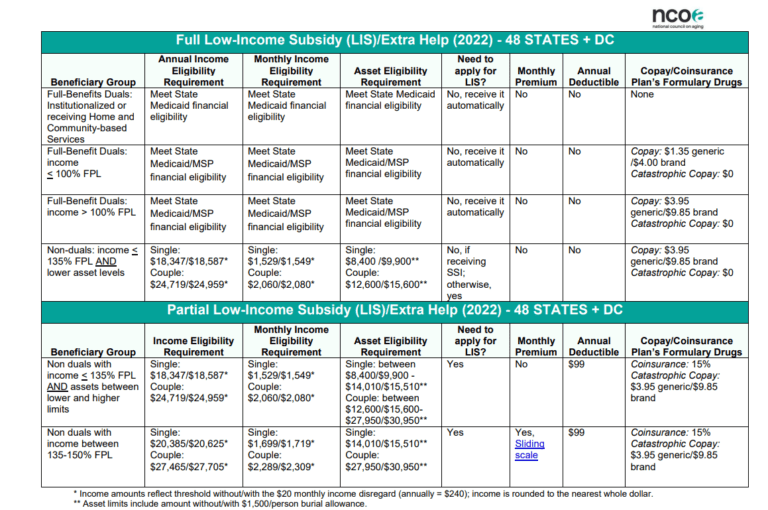
Extra Help benefit levels are broken down into two levels of help. These levels are Full Low-Income Subsidy and Partial Low-Income Subsidy, and both levels of Extra Help have a sliding scale of assistance within them. Both Full and Partial subsidies eliminate the Part D coverage gap, as well as any Part D Late enrollment penalties.
Full Low-Income Subsidy is for those with lower income and fewer resources. These include people that qualify as full-benefit duals or non-duals that have an income of less than or equal to 135% of the FPL and have lower asset levels. Full subsidy has no Part D plan premium, no Part D deductible, no co-pay during catastrophic coverage, and their regular copays are dependent on their income in relation where their income level is to the FPL. If their income falls between 135% FPL and 100% FPL then their prescription drug copays for 2022 are $3.95 for generic and $9.85 for brand-name drugs. If their income falls below 100% FPL, then their copays for 2021 are $1.35 for generic and $4.00 for brand-name drugs.
Partial Low-Income Subsidy is for those with slightly higher income and levels of resources than full subsidy, but still fall below 150% FPL. Partial subsidy also has a sliding scale depending on their income and resources in this level. Those who qualify for Partial Extra Help have no premium or a sliding scale premium (based on income), pay a $92 deductible, and have a 15% coinsurance for plan covered drugs. These numbers are based on 2021 subsidy levels. Refer to the graph below for more information.
Enrollment options and periods with LIS/Extra Help
Since people who qualify for Extra Help are receiving assistance with their Part D out-of-pocket costs, the LIS savings apply to both Part D Prescription Drug Plans (PDP) AND Medicare Advantage Plan with Part D (MAPD) so they can enroll in either. Qualifying for any level of Extra Help allows them to enroll or change plans outside of Medicare’s Annual Election Period (AEP). Using a Special Election Period, beneficiaries who qualify for LIS can make a change once each quarter during the first 3 quarters of the year. These are the 3 quarters outside of AEP. A change for any given quarter is based on the submission date, and not the effective date for the quarter. So, if a beneficiary submits an enrollment application for a plan change in April with a May 1st effective date, then they would have to wait until July to submit a new enrollment application with an August 1st effective date. They can also make a change during AEP with an effective date of January 1st.
Aside from these quarterly changes, they can also add or change a plan if they have any change in their LIS status. This includes if they lose eligibility, gain eligibility, or if their eligibility level moves up or down the previous mentioned benefit levels.
Helping Low-income clients
Many people who can qualify for Extra Help/LIS are not receiving the benefit. They either do not realize they may qualify or are not aware of the program. When meeting with clients, it is always good practice to know how Extra Help works, how to apply, as well as the LIS subsidy levels, including income and asset maximums so you can inform your clients and help them apply. This is a big benefit to people with low or limited income and resources that will help them make their income go further and get more treatment they couldn’t afford.
To learn more about how to reach and market LIS beneficiaries year for year round enrollments, check out “How to Market and Grow your Medicare Business with LIS and MSP Eligible Beneficiaries.”
Feel free to contact us and learn more about how we can help you and your agency.

2 Responses